You are never alone. Not even when you might want to be. Tucked away within the ~100m
2 of your bowels are ~10
14 (there are ~10
13 somatic and germinal cells in the human body) of your closest friends, collectively termed The Microbiota. They eat, spawn, conjugate, die, poop, fight, and secrete right there inside of you, unseen and mostly unthought of except when something is wrong. This system, the remarkably homeostatic mammalian gut, forms what is perhaps the densest and most complex microbial ecology on this planet.
These teeming microbes are not mere freeloaders living off of your access at their own convenience, they are true symbionts. In exchange for a warm, wet home and nutritional supply, they break down starches for us, metabolize complex molecules, and synthesize some key compounds, such as Vitamin K. It has been found that gnotobiotic, or germ-free, animal models require ~30% more calories to develop normally without a microbiota to help them out. In humans that have been on a broad-spectrum antibiotics, hardier inhabitants (such as
Clostridium difficile) can bloom when all of their more sensitive neighbors (such as
Bacteroides spp. and
Bifidobacterium spp.) are killed off, which causes very unpleasant colitis and diarrhea, that can then be cured by a transplant of fresh microbiota from a healthy individual (colloquially referred to as "poop soup"). Microbiome transplants can also transfer physiological characteristics from one individual to another. For example, the microbiomes of obese individuals have been found to have reduced numbers of Bacteroidales spp., and transfer of these microbiota via poop soup into germ-free mice resulted in obese mice, theoretically because these microbiota were more efficient at releasing calories from food.
Microbes exist, or can exist, in virtually every segment of the gastrointestinal tract from mouth to anus. In the mouth, a variety of
Actinomyces spp. are associated with the formation of plaque. In the forbidding and harsh environment of the stomach, only
Helicobacter pylori can thrive (it does so by hiding among the mucous lining the stomach and modulating the host immune response) and it has been found to directly cause stomach ulcers and has been further implicated in the formation of gastric cancers (it's the only organism classified as a BSL 2+ carcinogen). The proximal portion of the small bowel is relatively sparsely colonized at ~10
4-10
5 microorganisms/ml lumenal contents, which contrasts sharply with the densely colonized colon (~10
10-10
12 microbes/ml contents).
In the human and other mammals, diverse and distinct microbial ecologies also exist in the sinuses, ears, genitourinary tract (largely
Lactobacillus spp. in the vagina; the bladder is generally only colonized in disease states [long-term catherization and/or pyelonephritis] by uropathogenic
Escherichia coli,
Proteus mirabalis, et al), and on the skin as a whole (mostly
Staphylococcus spp.). These others will, however, be excluded from the present discussion.
However, what's very puzzling about all of this is: how does the mammalian immune system manage to differentiate from the massive basal antigenic signals coming from the microbiome from pathogenic antigens? In other words, why isn't the immune system raging against the huge number of microbial signals in the gut?
One of the exquisitely elegant features of normal gut physiology is that gut-associated lymphatic tissues (GALTs) mediate fine-tuned hyporesponsiveness to commensal microbiota while remaining responsive to pathogenic microbes. This flies directly in the face of most immunology, which holds that microbial antigens will always provoke a stimulatory response when ligated to TLRs, CLRs, or NODs (conserved receptors of the immune system that bind conserved molecular patterns associated with pathogens).
In vitro data support this. Physiology doesn't.
Physiologically, the germ-free mouse is weird. A germ-free animal is one that has been reared in an environment completely free of all microbes, fungi, and exogenous viruses and as such they have no native intestinal microbiota. Not only do they require more calories and vitamin supplementation, but they also tend to accumulate undigested fibrotic material in their ceca, which predisposes them to gut twists and bloat. Additionally, they feature underdeveloped Peyer's patches (distinct GALT sites on the gastric mucosa), altered CD4+ T-cell and IgA-producing B-cell population profiles, and the follicles in the spleen and lymph nodes where T- and B-cells mature are poorly formed. All of these abnormalities can be rescued by adding back microbial signals such as LPS, even without the microbes themselves. Due to these alterations, it is becoming accepted that the microbiome plays a crucial role in the normal development of the immune system. But to reconcile this with the dogma of microbial signal + PRR ---> inflammatory immune reaction is somewhat difficult, or at the very least complex.
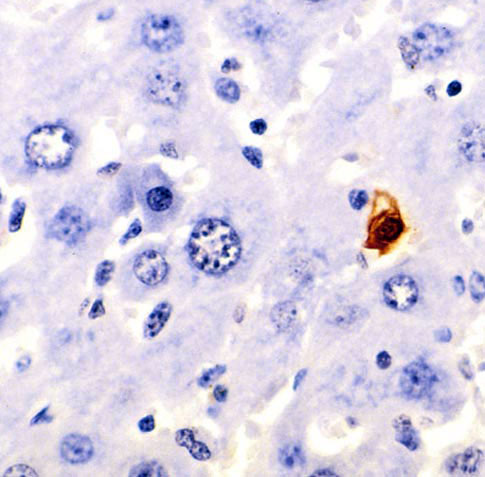
Immune cells that reside in the lamina propria underneath the gastric epithelium generally show signs of recent activation and a particular subset of dendritic cells (CX3CR1+) has been found to extend dendritic processes up through the tight junctions binding gastric columnar epithelial cells together to directly sample the lumenal contents. M cells that cap the Peyer's patches have been found to shuttle lumenal contents, and any antigens contained therein, to the dendritic cells and lymphocytes underneath. These pathways of antigen exposure are thought to be involved in the induction of immunological tolerance to microbiotal antigens, which could explain why the immune system does not attack the commensal microbiota. However, it does not explain how pathogen antigens processed by the same pathways are recognized as pathogenic and stimulate the immune system to attack.
Recent evidence strongly suggests that the intestinal epithelium itself is responsible for the differentiation of nonpathogenic microbiota from pathogens. Canonically, the intestinal epithelium is thought of as a simple barrier that is involved in the absorption and transcytosis of metabolites and nutrients. But it seems that it is much more involved that we had previously believed.
It turns out that intestinal epithelial cells (IECs) express TLRs and directly modulate the composition of the microbiome itself as well as the responsiveness of immune cells. This ranges from TLR expression on Paneth cells in the small intestine that secrete potent antimicrobial molecules (RegIIIg) when ligated [Dr. Lora Hooper, in seminar given 11/19/08] to
actual expression of MHCII and direct antigen presentation. It was previously believed that MHCII expression was restricted to antigen presentation by dendritic cells.
When investigators deleted TLR4, NOD1, or MyD88 (an adapter protein involved in many TLR-mediated NF-kB inflammatory pathways) in murine IECs they found that the mice were more susceptible to bacterial infections, which implies that the TLR signalling on the IECs is essentially to the development of normal protective immunity. A second feature of this is that IEC TLRs and NODs are located intracellularly, instead of on the cell surface as in immune cells, which means that they'd only be ligated and activated when an invasive pathogenic microbe breaks into the IECs themselves (e.g.,
Salmonella typhimurium,
Vibrio cholerae) as opposed to the more peaceful commensals. It may be that noninvasive gastrointestinal pathogens are recognized by the proteins that they shoot into IECs via Type IV secretions systems (e.g., Tir and
Escherichia coli O157:H7) in the same manner.
The commensal microbiota is also at work on the IECs themselves, actively acting against IEC-mediated inflammation.
Bacteroides thetaiotaomicron has been found to induce the PPARg anti-inflammatory (acts by increasing cytoplasmic shuttling of pro-inflammatory NF-kB away from the nucleus) mechanism in vitro. Commensal-derived metabolites such as butyrate (a short-chain fatty acid) have been found to inhibit expression of pro-inflammatory cytokines and increase expression of anti-inflammatory cytokines in IECs.
It is now thought that IECs regulate dendritic cell function through secretion of thymic stromal lymphopoietin (TSLP) and modulate T-cell activity through expression of MHCII in the abscence of costimulatory molecules. TLSP acts directly on dendritic cells and inhibits their production of pro-inflammatory cytokines (such as IL-12), which in turn promotes dendritic-cell-mediated activation of regulatory T-cells. TSLP is also implicated in skewing the immune response to a T
H2-type T-cell response, which is implicated in both response to metazoan parasites and pulmonary atopy. If naive T-cells are being exposed to MHCII on IECs without co-stimulatory molecules, then the T-cells will either kill themselves off (anergy) or mature into tolerogenic T-cells that limit the immune response to those given antigens. This, combined with widespread TGFb secretion by IECs, directly indicates an active role for IECs in promoting immune system hyporesponsiveness to the antigens present in the gastrointestinal system. Without this direct suppression of active, inflammatory immune responses, the immune system would be in a continual inflammation state due to not knowing what to do with a safe commensal antigen vs. a dangerous pathogenic antigen. Indeed, emerging research indicates that dysregulation of this process may underlie the pathophysiologies of inflammatory bowel disease and Crohn's disease.
It'll be interesting to see what's found next.
Artis, D. (2008). Epithelial-cell recognition of commensal bacteria and maintenance of immune homeostasis in the gut Nature Reviews Immunology, 8 (6), 411-420 DOI: 10.1038/nri2316