It’s a beautiful spring day, the first warm and sunny day of the year and the snow has finally melted. So naturally, you’re outside, enjoying it. The birds have reemerged from their hiding places, and all the plants are heavy with green and bloom. The whole earth smells clean, as though the snow and sleet somehow scrubbed the very grass and have made it shine, even if it is still brown and crinkles underfoot. Off in the birdsong distance, you can see the tree boughs tossing in the breeze. After so long cooped up inside with nothing but TV and the Internet, you ignore it. But then you suddenly notice that you’re struggling to pull air into your lungs while the air trapped deep inside is beginning to burn. You try to form words for help, yet nothing but a faint wheezing gasp comes out as you can literally feel your throat closing around your words like a wet, desperate fist. At this point you’re hunched over, chest heaving, desperate to yank the slightest bit of oxygen into your lungs that feel like a wet towel tightening slowly around your wildly beating heart. You clutch at your throat and a detached piece of your rapidly dizzying mind notices that your hands are shockingly cold. The crinkly grass rushes up and catches you as you strain, tendons taut and eyes watering, for any breath at all, barely enough of you left to wonder where you left your inhaler. But it’s there, digging into your hip in the pocket of your coat. Your lizard brain swats what remains of consciousness aside, manages to feebly flop you over, dig the inhaler out, and jam it between bluing lips. That first puff hits your throat cold and gritty, but it opens a little, just a bit, enough for the tiniest of breaths, which stings like salt. The second puff gets you going a bit more, and finally a third puff gets at least 1 bronchiole knocked wide open. Spreadeagled and panting hard on the grass, you watch the clouds scud above and silently curse the Ur-flower that first thought to make pollen. What a motherfucker that little bitch was. But at least you’re alive to even curse it.
***
Although we know quite a bit about the gross pathophysiology of asthma and, in most cases, how to treat it (acute and prophylactic), there remains quite a bit we do not know*. And there have been several well publicized epidemiological studies over the past 2 decades that indicate that asthma and allergy are increasing in prevalence across all socioeconomic lines. And the challenging and perhaps most frustrating part (and this, to me at least, is what makes it so intriguing) is that no one really knows why asthma and allergy (referred to together as atopy) are increasing, although we have hypothesizes ranging from diet, the hygiene hypothesis, perturbed gut microbial ecology, and general organic and synthetic chemical pollution.
First, let’s talk about the structural physiology of lungs. Anyone who has ever dissected a mouse knows that the lungs collapse into a wet pink mess pretty much as soon as the organism dies. This is because mice have spongy lungs (as opposed to “simpler” bag-like lungs in many animals) like humans. This is also because lungs are mostly soft tissue with air-filled tubes running throughout, somewhat analogous to Jello with holes drilled through it (though I don’t know why anyone would drill holes in Jello, if it’s even drillable [I may need to empirically test this]). The trachea branches off into the main bronchi, which each branch into lobar bronchi. These then branch into tertiary bronchi and form bronchopulmonary segments separated by connective tissue (lobes, essentially). Inside the bronchopulmonary segments the bronchi are called segmental bronchi, which then divide into primary bronchioles before dividing further into terminal bronchioles. And because this isn’t yet enough (think about it: each stage of segmentation increases the surface area per given unit volume quite efficiently, like a Sierpinski triangle), the terminal bronchioles branch into respiratory bronchioles branch into alveolar ducts end in alveolar sacs that contain the alveoli. Alveoli are where gas exchange happens via the blood vessels that cover most of their surface area. As the airways branch further out, rigid supporting cartilage decreases and smooth muscle increases. This is important to note for later, as are the observations that each lung does not branch perfectly symmetrically.
 Figure A: 2 ways to visualize the branching of the bronchi. Mandelbrot set visualization (top) and fractal tree (bottom).
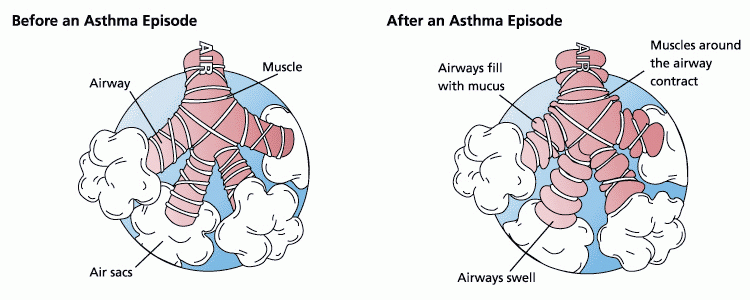
Figure A: 2 ways to visualize the branching of the bronchi. Mandelbrot set visualization (top) and fractal tree (bottom).Second, let’s talk about the pathophysiology of asthma. The possible causes and/or triggers of asthma warrant an entire series of posts by themselves, so they won’t be discussed here. Asthma occurs when the lungs aren’t providing adequate respiratory exchange due to constricted air flow volume (also referred to as tidal volume) and the levels of oxygen in the blood begin to fall; asthma is generally treatable with drugs, this is what clinically differentiates asthma from COPD and/or some ARDS. Reduced tidal volume is primarily thought to be a direct consequence of increased smooth muscle activation. Smooth muscles can be triggered by a wide variety of extrinsic factors and the resulting asthma attack can range from mild wheezing to complete respiratory failure and death. Long-term pathophysiological manifestations include scarring of the lung airway epithelium, localized sustained inflammation, and a reduced baseline tidal capacity, which are thought to be due to recruitment of immune system effector cells into the underlying tissues (which in turn cyclically drives more inflammation).
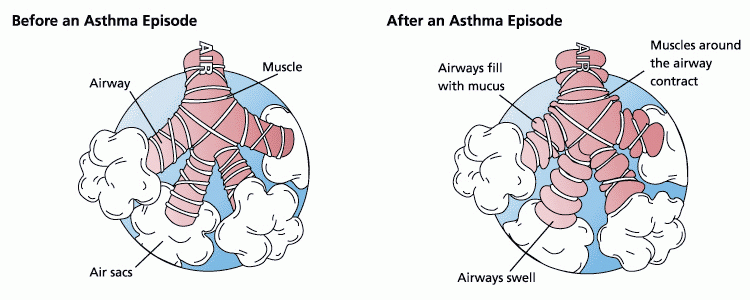 Figure B: Like that (although this .png has been squished a bit).
Figure B: Like that (although this .png has been squished a bit).
Finally, then, to the paper. A computational model of a single terminal bronchiole that included the physics of positive airway pressure inside the lumen space, the tension of underlying parenchymal upon bronchioles, and the constriction caused by smooth muscle activation was integrated to simulate a whole lung by using a Mandelbrot-like structure that reflects the serial branching of airways. This model assumes constant tidal volume and rate and neglects gravity-dependent lung effects as would occur in the deeper lungs. It also ignores the effect of diaphragm muscles on lung function. Obviously, in real life we breathe harder when we’re winded and the air deep in our lungs has to contend with gravity more than air in our upper lungs, and we also use muscles to breathe, but simplifications are necessary to make modeling a sane endeavor.
And now for the metaphorical vehicle: Imagine you’re standing on a tightrope with someone else at some distance away from you, say, farther than you could throw a tuba. If you lose your balance, you’ll swing about to try to regain it, and doing so will move the rope you’re standing on, which will then result in the other person having to move to keep their balance. If you don’t quickly recover your balance and steady the rope, either you’ll fall or the other person will have to work harder to stay on the rope and continue to amplify your instability.
 Figure C: Don't try this at home. Go somewhere more dangerous first.
Figure C: Don't try this at home. Go somewhere more dangerous first.Unfortunately, falling off the rope doesn’t really happen in asthma attacks (unless you think of that as a piece of lung shutting down). Sure, whole chunks of lung seize up and stop providing adequate ventilation, but this is patchy and even then those patches still contain smaller bits that still work as they’re supposed to. But it is the amplification of instability that leads to the progressive and terrifyingly fast clamping shut of airways in an asthma attack. Section A shuts down, so Sections B, C, and D will have to work harder to compensate. Compensation will involve greater intrabronchial airway pressure, which the normally functioning lung interprets as bad and tries to compensate for in the opposite direction by activating smooth muscle, so smooth muscle activation and airway constriction can spread rapidly from Section A to B to C in sudden and catastrophic sequence even if only a little tiny bit of Section A started the whole thing.
The computational model used in this paper found that catastrophic shifts as described above don’t really happen unless some degree (~1%) of heterogeneity in lung response to constriction/smooth muscle activation is included. If the computational model was allowed to be completely symmetrical and if all lung tissue responded in exactly the same way, then nothing spectacular happened.
While I find the computational modeling stuff to be fascinatingly awesome, that’s not all they did. They also got mild to moderate asthmatic volunteers to inhale isotopic nitrogen gas inside of a PET machine during a chemically induced asthma attack to map where the gas was going (those were very brave asthmatics). In poorly functioning lung, iN2 would be trapped and remain visible on the PET while normally functioning, or lung hyper-functioning to compensate, lung would clear it quickly. These PET results validated their modeling outcomes in that asthmatic events are patchy in that neighboring bronchioles are more likely to become distressed than distant bronchioles, though not absolutely in that the patchiness of poorly ventilated lung was itself patchy (mirroring computationally induced heterogeneity). Furthermore, these findings were clinically relevant because only normal- or hyper-functioning lung remained open during the asthmatic event, which suggests that inhaled anti-inflammatories may be being delivered primarily to the lung epithelium that needs it least.
Research Cited:
Jose G. Venegas, Tilo Winkler, Guido Musch, Marcos F. Vidal Melo, Dominick Layfield, Nora Tgavalekos, Alan J. Fischman, Ronald J. Callahan, Giacomo Bellani, R. Scott Harris (2005). Self-organized patchiness in asthma as a prelude to catastrophic shifts Nature, 434 (7034), 777-782 DOI: 10.1038/nature03490
*From my perspective as someone who doesn't actually do atopy research...yet, anyway. Therefore, if I am flatulating ignorance and posing it as wisdom, feel free to correct my mistakes in comments.
NOTE: This is my first post for the Cyber Journal Club that Science Bear is organizing. R.E.S.E.A.R.C.H.E.R.S are also participating. My goal is to post every Wednesday and apparently Science Bear is going to be posting 2 Wednesdays a month. Feel free to join in by commenting or posting your own (we'll ping you).