***
Although we know quite a bit about the gross pathophysiology of asthma and, in most cases, how to treat it (acute and prophylactic), there remains quite a bit we do not know*. And there have been several well publicized epidemiological studies over the past 2 decades that indicate that asthma and allergy are increasing in prevalence across all socioeconomic lines. And the challenging and perhaps most frustrating part (and this, to me at least, is what makes it so intriguing) is that no one really knows why asthma and allergy (referred to together as atopy) are increasing, although we have hypothesizes ranging from diet, the hygiene hypothesis, perturbed gut microbial ecology, and general organic and synthetic chemical pollution.
First, let’s talk about the structural physiology of lungs. Anyone who has ever dissected a mouse knows that the lungs collapse into a wet pink mess pretty much as soon as the organism dies. This is because mice have spongy lungs (as opposed to “simpler” bag-like lungs in many animals) like humans. This is also because lungs are mostly soft tissue with air-filled tubes running throughout, somewhat analogous to Jello with holes drilled through it (though I don’t know why anyone would drill holes in Jello, if it’s even drillable [I may need to empirically test this]). The trachea branches off into the main bronchi, which each branch into lobar bronchi. These then branch into tertiary bronchi and form bronchopulmonary segments separated by connective tissue (lobes, essentially). Inside the bronchopulmonary segments the bronchi are called segmental bronchi, which then divide into primary bronchioles before dividing further into terminal bronchioles. And because this isn’t yet enough (think about it: each stage of segmentation increases the surface area per given unit volume quite efficiently, like a Sierpinski triangle), the terminal bronchioles branch into respiratory bronchioles branch into alveolar ducts end in alveolar sacs that contain the alveoli. Alveoli are where gas exchange happens via the blood vessels that cover most of their surface area. As the airways branch further out, rigid supporting cartilage decreases and smooth muscle increases. This is important to note for later, as are the observations that each lung does not branch perfectly symmetrically.
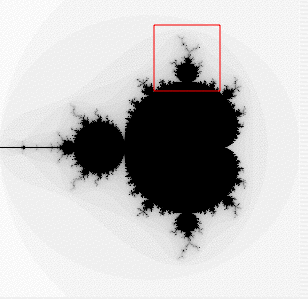
 Figure A: 2 ways to visualize the branching of the bronchi. Mandelbrot set visualization (top) and fractal tree (bottom).
Figure A: 2 ways to visualize the branching of the bronchi. Mandelbrot set visualization (top) and fractal tree (bottom).Finally, then, to the paper. A computational model of a single terminal bronchiole that included the physics of positive airway pressure inside the lumen space, the tension of underlying parenchymal upon bronchioles, and the constriction caused by smooth muscle activation was integrated to simulate a whole lung by using a Mandelbrot-like structure that reflects the serial branching of airways. This model assumes constant tidal volume and rate and neglects gravity-dependent lung effects as would occur in the deeper lungs. It also ignores the effect of diaphragm muscles on lung function. Obviously, in real life we breathe harder when we’re winded and the air deep in our lungs has to contend with gravity more than air in our upper lungs, and we also use muscles to breathe, but simplifications are necessary to make modeling a sane endeavor.
And now for the metaphorical vehicle: Imagine you’re standing on a tightrope with someone else at some distance away from you, say, farther than you could throw a tuba. If you lose your balance, you’ll swing about to try to regain it, and doing so will move the rope you’re standing on, which will then result in the other person having to move to keep their balance. If you don’t quickly recover your balance and steady the rope, either you’ll fall or the other person will have to work harder to stay on the rope and continue to amplify your instability.
Unfortunately, falling off the rope doesn’t really happen in asthma attacks (unless you think of that as a piece of lung shutting down). Sure, whole chunks of lung seize up and stop providing adequate ventilation, but this is patchy and even then those patches still contain smaller bits that still work as they’re supposed to. But it is the amplification of instability that leads to the progressive and terrifyingly fast clamping shut of airways in an asthma attack. Section A shuts down, so Sections B, C, and D will have to work harder to compensate. Compensation will involve greater intrabronchial airway pressure, which the normally functioning lung interprets as bad and tries to compensate for in the opposite direction by activating smooth muscle, so smooth muscle activation and airway constriction can spread rapidly from Section A to B to C in sudden and catastrophic sequence even if only a little tiny bit of Section A started the whole thing.
The computational model used in this paper found that catastrophic shifts as described above don’t really happen unless some degree (~1%) of heterogeneity in lung response to constriction/smooth muscle activation is included. If the computational model was allowed to be completely symmetrical and if all lung tissue responded in exactly the same way, then nothing spectacular happened.
While I find the computational modeling stuff to be fascinatingly awesome, that’s not all they did. They also got mild to moderate asthmatic volunteers to inhale isotopic nitrogen gas inside of a PET machine during a chemically induced asthma attack to map where the gas was going (those were very brave asthmatics). In poorly functioning lung, iN2 would be trapped and remain visible on the PET while normally functioning, or lung hyper-functioning to compensate, lung would clear it quickly. These PET results validated their modeling outcomes in that asthmatic events are patchy in that neighboring bronchioles are more likely to become distressed than distant bronchioles, though not absolutely in that the patchiness of poorly ventilated lung was itself patchy (mirroring computationally induced heterogeneity). Furthermore, these findings were clinically relevant because only normal- or hyper-functioning lung remained open during the asthmatic event, which suggests that inhaled anti-inflammatories may be being delivered primarily to the lung epithelium that needs it least.
Research Cited:
Jose G. Venegas, Tilo Winkler, Guido Musch, Marcos F. Vidal Melo, Dominick Layfield, Nora Tgavalekos, Alan J. Fischman, Ronald J. Callahan, Giacomo Bellani, R. Scott Harris (2005). Self-organized patchiness in asthma as a prelude to catastrophic shifts Nature, 434 (7034), 777-782 DOI: 10.1038/nature03490
*From my perspective as someone who doesn't actually do atopy research...yet, anyway. Therefore, if I am flatulating ignorance and posing it as wisdom, feel free to correct my mistakes in comments.
NOTE: This is my first post for the Cyber Journal Club that Science Bear is organizing. R.E.S.E.A.R.C.H.E.R.S are also participating. My goal is to post every Wednesday and apparently Science Bear is going to be posting 2 Wednesdays a month. Feel free to join in by commenting or posting your own (we'll ping you).








2 comments:
Great background info! I am getting ready for 2 exams and a paper all due in the next 6 hours, but will be eagerly anticipating providing some input this evening!
I particularly liked the background before getting to the meat of what the paper was about, since it helps explain the anatomical position of interest and why we are interested in that area! I was always introduced to the anatomy of the lungs as an inverted tree, for the visual divergence of the system (very visual learner).
Asthma is one of the things we used to look at in my lab, but now the focus has shifted slightly.. i.e. the student who did most of that research graduated.
Love the addition of the figures!
Post a Comment